Medical billing and coding play a crucial role in the healthcare industry by ensuring accurate reimbursement for healthcare services. This article delves into the intricacies of this field, focusing on mastering the language of healthcare reimbursement.
By understanding the basics of medical terminology and navigating through complex billing codes, professionals in this field can ensure that providers, insurance companies, and patients receive fair and accurate compensation.
The impacts of medical billing and coding on various stakeholders will also be explored.
The Role of Medical Billing and Coding in Healthcare
The role of medical billing and coding in healthcare is to accurately translate medical procedures and diagnoses into codes for reimbursement purposes. This process is integral to the revenue cycle of healthcare organizations as it ensures that healthcare providers are appropriately compensated for their services.
Medical coders and billers use standardized code sets, such as the International Classification of Diseases (ICD) and Current Procedural Terminology (CPT), to assign codes to various healthcare procedures and diagnoses. These codes serve as a common language between healthcare providers, insurance companies, and government agencies, facilitating accurate reimbursement for services rendered.
Moreover, medical billing and coding play a crucial role in maintaining accurate healthcare documentation. By translating complex medical information into standardized codes, this process helps ensure consistency, accuracy, and completeness in patient records, enabling effective communication among different stakeholders involved in the delivery of care.
Understanding the Basics of Medical Terminology
Understanding the basics of medical terminology involves familiarizing oneself with the language used in healthcare documentation. Medical terminology consists of specific terms and definitions that are essential for effective communication in the field of healthcare. These terms are used to describe various aspects of the human body, diseases, diagnoses, procedures, and treatments.
Additionally, medical abbreviations play a crucial role in medical terminology as they help to convey information quickly and efficiently. However, it is important to note that these abbreviations can vary between different healthcare settings and specialties. Therefore, it is imperative for medical billing and coding professionals to have a comprehensive understanding of both the common medical terminologies and abbreviations used in their respective fields.
Mastering this aspect of healthcare language is vital for accurate documentation and efficient reimbursement processes.
Navigating the Complex World of Billing Codes
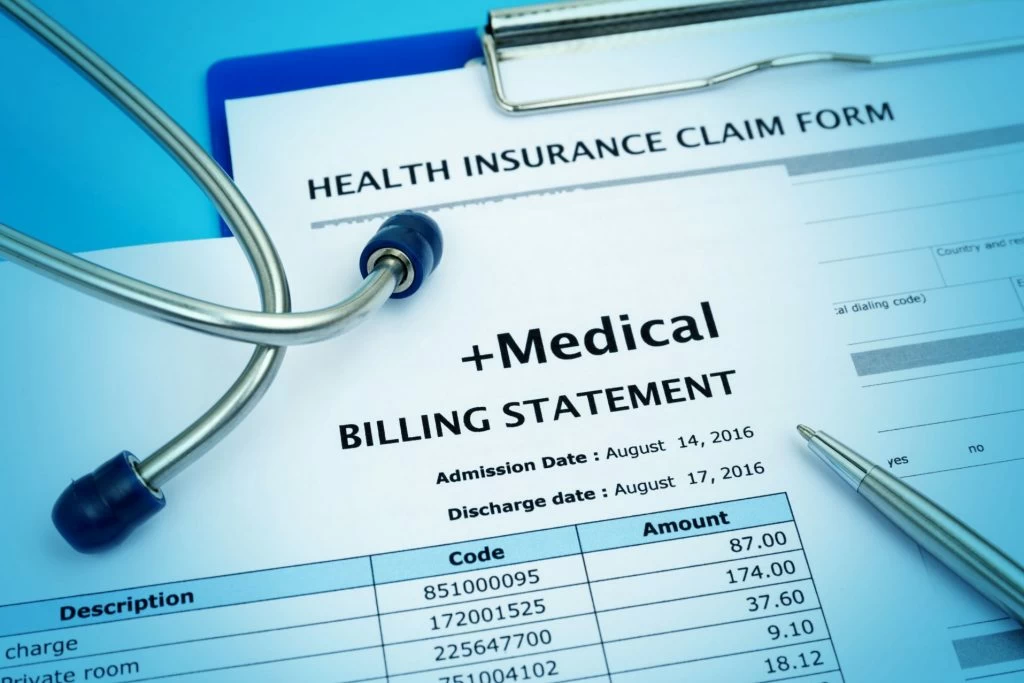
Navigating the complex world of billing codes requires a comprehensive knowledge and understanding of the various coding systems used in healthcare documentation. A billing system is a crucial component of the healthcare reimbursement process, as it ensures accurate and timely payment for services provided.
Coding guidelines play a vital role in this process by providing specific instructions on how to assign appropriate codes to medical procedures, diagnoses, and treatments. These guidelines ensure consistency and accuracy across different healthcare settings, allowing for effective communication between providers, insurance companies, and government entities.
Additionally, coding guidelines help prevent fraud and abuse by ensuring that claims are properly documented and coded. Mastering these coding systems and guidelines is essential for medical billers and coders to accurately translate medical information into universally understood language for reimbursement purposes.
Ensuring Accurate Reimbursement for Healthcare Services
Achieving precise and timely compensation for healthcare services requires adherence to accurate coding systems and guidelines. Reimbursement challenges can arise when healthcare providers fail to accurately code the services they provide.
Accurate coding is crucial because it ensures that the correct amount of reimbursement is received based on the complexity and nature of the healthcare service rendered. Inaccurate coding can result in underpayment or overpayment, leading to financial losses for both providers and payers. Furthermore, it can also impact patient care by delaying or denying necessary treatments due to inadequate reimbursement.
To ensure accurate reimbursement, healthcare providers must stay up-to-date with coding updates, guidelines, and regulations. Regular training and auditing processes can help identify any potential errors or inconsistencies in coding practices, improving overall accuracy in billing and facilitating fair compensation for healthcare services provided.
Impacts of Medical Billing and Coding on Providers, Insurance Companies, and Patients
The impacts of accurate and timely documentation and categorization of healthcare services extend to healthcare providers, insurance companies, and patients alike. Proper medical billing and coding practices have a significant impact on healthcare costs. When healthcare services are accurately categorized, it enables insurance companies to determine the appropriate reimbursement amounts for providers. This helps prevent overbilling or underbilling, which can lead to financial losses for both parties involved. Accurate documentation also ensures that patients are billed correctly, preventing them from being burdened with unnecessary expenses.
However, implementing effective medical billing and coding practices can be challenging. Healthcare providers face the task of staying updated with ever-changing coding guidelines and regulations. Compliance with these guidelines requires continuous education and training for staff members involved in the billing process. Additionally, there may be discrepancies between different insurance companies’ reimbursement policies, leading to further complexities in the implementation of medical billing and coding practices.
Overall, accurate medical billing and coding have far-reaching impacts on healthcare costs while presenting challenges in their implementation due to evolving regulations and varying reimbursement policies among insurance companies.
Technological Advancements and Their Influence on Medical Billing and Coding
In recent years, the landscape of medical billing and coding has been significantly reshaped by technological advancements. Electronic Health Records (EHR) systems have revolutionized the way patient information is stored, accessed, and communicated, streamlining billing processes and reducing manual errors. Artificial Intelligence (AI) and machine learning tools are now being integrated into billing software to identify discrepancies, anticipate claim denials, and suggest corrective actions.
Automation tools expedite coding tasks, allowing coders to focus on complex cases that require human expertise. Bockchain technology is emerging as a potential solution for ensuring data integrity and combating fraud in medical billing. With these advancements, the industry faces new challenges such as adapting to rapid technological changes and ensuring staff are adequately trained. Nonetheless, the potential for improved efficiency, accuracy, and transparency in the billing and coding process is unprecedented, paving the way for a more streamlined healthcare reimbursement system.









